Medicaid Managed Care
Medicaid managed care (MMC) is a health care delivery system organized to manage cost, utilization, and quality and is a common mechanism for financing health care services for CYSHCN. MMC programs deliver physical and behavioral health benefits along with additional services through contractual arrangements between state Medicaid programs and managed care organizations (MCOs) through a set per member per month (PMPM) payment for services.
Diving In
The structure of state Medicaid managed care models varies by state. Complete this worksheet to learn more about Medicaid Managed Care Organizations in your state.
MMC Procurement Process
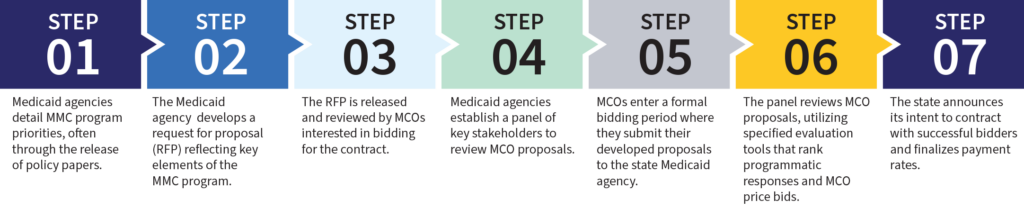
MMC procurement process is the process by which state Medicaid agencies solicit bids from one or more MMC organizations, and then contract with the ones that meet their requirements to provide services to Medicaid beneficiaries in the state. Engagement in the MMC procurement process can be an important way for Title V to contribute their subject matter expertise to the design of a MMC program, support the alignment of Title V and Medicaid mutual goals and priorities, and improve the system of services for CYSHCN. These steps are essential to the MMC program procurement process.
MMC Procurement Process Steps
Step 1: Medicaid Agencies Detail MMC Program Priorities, Often Through the Release of Policy Papers.
North Carolina issued a series of policy papers as the state transitioned to a MMC model. The paper on their behavioral health and intellectual/development disability-tailored MMC program focuses on care coordination and delivering whole-person care to children with complex health conditions.
Step 2: The State Develops a Request for Proposals Reflecting Key Elements of the MMC Program.
A recent Minnesota RFP asked potential MCOs to detail strategies for connecting families to social supports as well as efforts to address structural racism within systems and processes.
Texas uses workgroups comprised of subject matter experts to develop the priorities and details of RFPs, including service coordination, continuity of care, behavioral health services, and quality measurement.
Step 4: Medicaid Agencies Establish a Panel of Key Stakeholders to Review MCO Proposals.
During the procurement process for Virginia’s largest MMC program called Medallion 4.0, the Medicaid agency invited Title V representatives to participate in the procurement review panel that selected the participating MCOs.


Equity Spotlight
Participating in the MMC procurement process is an opportunity to advance equity in your state by:
- Engaging interested parties to ensure that MCOs will meet the needs of CYSHCN
- Elevating the population-specific needs of CYSHCN in the design of managed care programs, including the needs of children in foster care
- Naming the roles of ableism in impacting health outcomes
- Emphasizing network adequacy for rural populations
MMC Quality Strategy
States are required by federal regulation 42 CFR § 438.340 to develop and maintain a quality strategy that assesses and improves the quality of MMC services. Requirements include the development of a state quality strategy and external quality review (EQR). Under this federal regulation, each state is responsible for submitting a copy of its quality strategy to CMS, along with regular reports on implementation and the effectiveness of the quality strategy. Many states also incorporate the CMS Medicaid/CHIP Child Core Set measures into their quality strategy.
The measures that states incorporate into their quality strategy can reflect the priorities of their program. Determining measures that reflect what’s important to families are an important opportunity to improve the system of services for CYSHCN.

Learn More About Title V's Role in Medicaid Managed Care
Tools, Templates, and Tips


